The following is the first part in a two-part installment.
Author Note: This article comes from a paper that was originally presented at the Critical Education in an Era of Crisis Conference, Thessalonkiki, Greece. It is the second of two. The first involved an analysis of pre-capitalist, indigenous models of health and critically compared these to our normative capitalist system. The first one was published previous in The New Polis. The first and second installments of that article can be found here and here.
“The most odious form of colonisation, and that which has brought with it the greatest pain for the colonised – (is) the colonisation of the mind.” – Frantz Fanon (1963)
“As Paulo Freire and Antonio Faundez wrote, indigenous knowledge is a rich social resource for any justice-related attempt to bring about social change. In this context, indigenous ways of knowing become a central resource for the work of academics… Intellectuals, Freire and Faundez conclude, should “soak themselves in this knowledge… assimilate the feelings, the sensitivity” of epistemologies that move in ways unimaginable to many Western academic impulses. …Only now, in the Twenty-first Century, are European peoples just starting to appreciate the value of indigenous knowledge(s) about health, medicine, agriculture, philosophy, spirituality, ecology and education.” – Joe Kincheloe (2007)
The Need for A New Model of Community Development
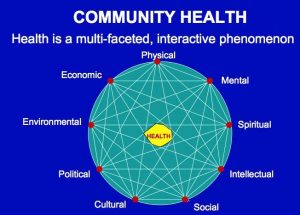
In my earlier article, I detailed the failure of the capitalist model regarding community health and development that is standard across the world, showing how it disempowers and destroys local communities as profits and resources are extracted from the community and appropriated into the private realm as governments cut services while simultaneously privatising essential resources. I developed a critical analysis of Western health systems and contrasted this with indigenous models that offer a more holistic and caring alternative from which we might learn. I suggested that we need to develop a radical redefinition of community health to include multiple factors as well as a radical restructuring of community power and self-determination.
This analysis came out of a project with which I have been involved, in the small New Zealand town of Whakatane, involving the development of a community hub – a facility initiated and operated by the community with the intention of reversing the appallingly negative statistics among the town’s youth and elderly. The worst of these statistics are attributable to the indigenous Māori population of the town (50% – almost four times the national average). Working in a bicultural context such as this provided insights into how we might approach the development and operation of this facility in ways that are replicable elsewhere.
This next part of the analysis describes the process by which we developed design proposals in collaboration with the community, together with detailed descriptions of the proposals themselves. The designs were carried out by a culturally diverse group of 24 second year architecture students (of eleven different nationalities), working with seven local high school students to successfully navigate the complex web of requirements and diverse social, cultural and economic needs of the community.
The students designed a family-friendly, universally accessible facility catering to the needs of all cultural groups, ages and beliefs. Key to the proposals was an understanding of the historical causes of the community’s difficulties, particularly the impact of colonisation on the Māori community and its implications for a program of self-determination and community control.
The Impact of Colonization
Captain James Cook “discovered” New Zealand in 1769, and there followed a period of increasingly frequent visits by sealers, missionaries and early settlers until, in 1840 a large number of Marri chiefs signed the Treaty of Waitangi with the British Crown – agreeing to the admission of British subjects in return for the protection of the Māori way of life and culture. Once signed, the Treaty was ignored by the new white New Zealanders, who embarked upon a ruthless policy of Māori land acquisition, until two centuries after Cook’s landing, Māori – an otherwise entrepreneurial race – had been dispossessed of 95% of their productive capacity.
The introduction of European missionary schools, with strict rules (until the 1960s) forbidding the use of Māori language, the suppression and execution of native leaders, and the creation of a Māori education system designed to produce service workers for the white elite all conspired to reduce Māori to a subordinated, compliant culture within their own land. Their spiritual beliefs and customs were suppressed, the traditional close family structures and tikanga (prohibitions) that had safeguarded members against sexual and/or family abuse were severed and replaced by a patriarchal system that, with the introduction of industrialization, saw the traditional extended Māori family structure shattered.
Not only did colonization reduce indigenous populations to state-dependency by destroying their organic social, political and spiritual systems, but also the imposition of the supposedly superior Western systems has simply compounded the problem, according to Lawson-Te Aho. In the New Zealand field of health, the process involved the outlawing and criminalization of Māoridom’s spiritual and health practitioners. The 1907 Tohunga Suppression Act specifically targeted traditional Māori healers (tohunga) and made the practice of traditional healing practices unlawful. The act was passed with the purpose of protecting the Māori community from introduced diseased like influenza and smallpox. Although there were only nine convictions under the act, nevertheless the result was that many tohunga refused to pass on their oral traditions and much traditional knowledge was lost.
Over time, many practices were driven underground, some to be passed on orally from generation to generation. But many were lost, and with the loss, the communities that had safeguarded their own health for hundreds of years were forced to accept commodified European models and practices. This is true in all spheres, from physical health to social and cultural health and family counseling.
The result of all of this was a sharp decline in personal and community Māori health, with increasingly disproportionate statistics in family violence, substance abuse and suicide. Family violence among indigenous communities is now epidemic around the world, including New Zealand. Domestic violence is a major issue in New Zealand and the cost to the nation is enormous. According to Infometrics, it has been estimated that child abuse alone costs the nation, both directly and indirectly over $2 billion a year, while family violence as a whole has been estimated to cost $8 billion a year in a population of barely 4 million, yet less than 0.1% of GDP per year is spent on preventive measures.
Furthermore, Stacey Kirk describes how incidence of family violence is increasing. In New Zealand, an over-representative proportion of this violence and its associated cost occurs in the Māori community, as detailed by Roma Balzer and associates. The primary victims are women and children. This is in stark contrast to traditional and harmonious pre-colonial gender relationships that were built into the cosmologies that guided communal life.
The Failure of Western Health Systems
Despite government concern over 25 years and the production of two major government reports, and despite years of investment and some measure of success locally, the problem of whanau (family) violence continues to be an area of major concern. Indeed, it has been noted that western systems of intervention and treatment are failing Māori, and have not curbed the epidemic of whanau violence. More to the point, Māori professional social workers have implicitly noted the ongoing colonialism of the system by observing that if whanau violence interventions continue to be delivered from a non-Māori conceptual and practice framework that isolates, criminalises and pathologies Māori individuals, nothing will change, according to Tamati Kruger and associates.
Key to this failure is the inability of the system to distinguish between the related concepts of whanau and family – the former including reference to past, present and future generations – including those of the colonial past, which could explain the roots of violence through the destruction of extended family relationship safeguards in traditional Māori society. The Western use of “family” tends, by comparison, to operate only in the present to deny colonial causality, while at the same time failing to recognise the importance of rebuilding these traditional relationships and the safeguards that they embodied, as noted by Fiona Cram.
This is a crucial point because it is precisely the imposition of colonial western models of the nuclear family that has destroyed the social and cultural safeguards against whanau violence that existed in traditional Māori society. The notion of whanau carries important meanings in terms of relationships of mutual responsibility and reciprocity – mutually safeguarding whanau members from violence and harm through an adherence to tikanga (customary tradition). In this sense, Mason Durie describes how violence within or against any whanau member was seen as a disturbance and imbalance of tikanga (tradition) that must be repaired and reinstated.
It is only when we consider the extent and impact of colonialism and the ongoing imposition of Eurocentric meanings within the health field that we can begin to understand the ways in which we perpetuate the ongoing colonisation and ill-health of subordinated cultures like Māori, and the absolute need to create the space for them to reclaim their own systems of care by rebuilding their tikanga and whakapapa connections. Self-determination is the sine qua non of community health, as well as of social transformation at the larger, global scale. This is something that our models of emerging socialism fail to grasp when they assume that the only requirement is the destruction (or withering away!) of the capitalist economic base. It is also something that explains the failure of many budding socialist revolutions to gain the support of indigenous communities like the Miskito in Nicaragua under the Sandinistas.
In addition to the confiscation of lands the destruction of whanau structures, the imprisonment and execution of native leaders and healers, the education system was structured into a two-tier system to educate Europeans to positions of leadership and Māori to work in the service industries. The fragmentation of Māori culture was achieved through land-loss and consequential urban drift to man the emerging industries of the new colony.
During the years following WW2, with the rise of socialist policies in health, housing, welfare and education in Britain, Australia, New Zealand and Canada, free social services became the norm, and the health, education and general welfare of families prospered. But for Māori, this prosperity came at the cost of some loss of identity as they were “assimilated” into the larger colonial culture, many losing their language, their connections to their geographical (turangawaewae) and cultural roots. The worldwide rise of indigenous independence movements that began in the 1940s, and which continues today, was a direct response to this loss, to the continuing appropriation of indigenous lands and resources and to the increasing disparities of wealth between themselves and the dominant (white) culture.
A Tale of Two Cities
Fortunately, the process of colonization was never completely successful, either in New Zealand or elsewhere in the colonial world, and many indigenous communities, including Māori, have retained at least some of their cultural identity and many of their cultural beliefs and practices down to the present time, and these may offer guidance in how we may all resist and confront market-driven ideologies to reclaim our community health. What follows is one experiment in this process of reclamation.
Despite some recent advances in their collective health, Māori remain at the bottom of all social health indices. Increasingly, they have taken matters into their own hands, demanding a degree of autonomy and self-determination from the “mainstream” state systems. In education, Māori have developed their own, culturally appropriate parallel system, and have taken a lead in administering the state health system with culturally appropriate practices. In the field of Māori health, a study by Ward in New Zealand promoted an alternative model of health that drew from Māori traditions in the design of a Māori community hospital. More recently, the model has been extended and improved, this time in the design of a small community facility in the author’s home-town of Whakatane.
This is a tale of two cities. The town is unique in many respects. It has one of the largest proportions of Māori residents (50% in the Eastern Bay) in the country and the highest per capita number of native language speakers. It is the “sunshine capital” of New Zealand, it has the country’s Best Beach Award and it is surrounded by some of the nation’s most remarkable fishing, hiking and recreational environments. But Whakatane is a divided community. If you are white, middle class and employed, it is a fantastic place to raise a family. If, on the other hand, you are Māori, and unemployed it can be the worst of places. Besides its positive attributes, it also has the nation’s worst statistics in a range of social parameters:
- Highest truancy rates
- Lowest academic achievement rates
- Among highest unemployment rates
- The second-highest child abuse rates
- Highest family violence rates
- Highest youth suicide rates (regionally)
- Among lowest income rates
- Increasing disparities in wealth, health and hope.
Many of these statistics are attributable predominantly to the 50% Māori community. The reasons for their contemporary social and cultural situation can be traced back to issues of 19th century land dispossession cited earlier. One of the primary means of land dispossession was “legal” confiscation. Under the New Zealand Settlement Act of 1863, tribes that were deemed “rebellious” had their land confiscated by the government. The definition of “rebellious” bore striking (and slippery) similarities to American Indian “Hostiles” and today’s “terrorists” – convenient labels for demonizing those we oppress. When provocative government raids of native lands were resisted by Māori tribes, they were labeled “rebellious,” their leaders imprisoned and hung, and their lands taken.
This was particularly onerous for the tribes of the Eastern Bay of Plenty (Ngati Awa, Whakatohea), who live in Whakatane and neighbouring Opotiki and who had their entire land holdings confiscated on the basis of fabricated charges of murder and sedition. Their lands were taken and their leaders were executed (and recently exonerated). The neighboring and related Tuhoe tribe were subject to a scorched-earth and occupation campaign by the government – all of this leaving a community of later bicultural generations down to our own time that would harbor barely disguised feelings of mutual antagonism and hatred which would be one of the key issues to be addressed by the project described here.
Documented by Judith Binney, these antagonisms were exacerbated in 1916, when the police mounted a dawn attack on the peaceful Tuhoe village of Munga Pohatu against the community of Rua Kenana (who had urged his followers to ignore the military draft for WW1), killing his son and imprisoned Rua for two years. Even as recently as 2005, in a raid reminiscent of that in 1916, the police mounted another dawn raid on the Tuhoe village of Ruatoki, breaking into houses, arresting many of the inhabitants and detaining women and children without food or water for 24 hours – all on the basis of trumped up “terrorism” charges that were later dropped.
 Reclaiming Community Health
Reclaiming Community Health
The legacy of these state oppressions has been to leave the small town of Whaktane a divided community – the historical roots of which are rarely recognised or addressed by social service agencies who, instead, frequently work through a deficit model of community well-being which only exacerbates the situation. The fact is, that the community has no facility or agency that operates biculturally – a place where Māori and non-Māori can come together in a collective process of healing. In the absence of such a facility, the town’s community health remained stubbornly poor.
In October 2011, facing serious breakdown in community health, two social service providers – Pou Whakaaro and Supporting Families – floated the idea of getting all of the town’s service providers to co-locate as a way of cutting costs, improving efficiency and referrals and making it easier for their clients to navigate the social service system.
Clearly the providers were facing a formidable set of conditions. What was clear was that the problem could not be solved with the status quo model of social service provision. Dealing with family violence, crime or truancy without dealing with unemployment, economic disparities, mental health issues, illiteracy or the breakdown of culturally appropriate whanau and whakapapa relationships had proven to be a waste of time and resources. That model was failing. What was required was a coordinated and multifaceted approach – a model of community health that embraced a wide range of factors responding to a wide range of community needs with referrals and interventions made seamless. Such a model would be built upon the principle of grass/flax root relationship-building of, by and for the community, available to everyone at a sustainable cost.
Following two provider workshops and a community-wide online survey, a pattern of social and cultural needs that were congruent with the provider aims began to emerge. The survey results revealed:
- bored and depressed youth
- lonely and depressed elderly
- adults with unmet social, economic and physical support needs
- unmet needs of numerous community groups
- a lack of coordinated transport and referral services
Responding to the survey questionnaire, the community itself recommended specific functional remedies that might be included in a more comprehensive Whakatane Community Hub facility:
| A Place to Hang Out | 64.2% | 217 |
| Computer Centre / Internet Access | 52.1% | 176 |
| A cafe w/ a child play area | 34.9% | 118 |
| Childcare | 12.4% | 42 |
| Community Garden | 33.4% | 113 |
| A place to play live music | 55.6% | 188 |
| Monthly open mural space | 18.0% | 61 |
| Free Shuttle bus to services | 40.5% | 137 |
| Dances | 28.7% | 97 |
| Cooking Space | 20.7% | 70 |
| Rock Climbing wall | 40.5% | 137 |
| Workshop space (art, yoga, weaving, budgeting, etc) | 42.3% | 143 |
| Linking to Community services | 28.1% | 95 |
| A place to learn how to use technology (computers, | 31.7% | 107 | |
| graphics, programs) | |||
| Commercial Kitchen (to make and sell cooked items) | 21.9% | 74 | |
| A place to get help | 33.1% | 112 | |
| Community BBQ’s | 32.8% | 111 | |
| Community Festivals | 46.2% | 156 | |
| Flea markets | 36.1% | 122 | |
| Central Booking place for area services, sites, resources | 21.3% | 72 | |
| Multi-Cultural celebrations | 27.8% | 94 | |
| Ten Pin Bowling | 55.9% | 189 | |
| Somewhere to exercise and stay fit | 38.2% | 129 | |
| A place to show and see special movies | 44.1% | 149 | |
| Somewhere to host a conference | 24.0% | 81 | |
| Other (you tell us) | 22.5% | 76 |
There were few discernible differences across age and ethnicity. Based upon all of these findings, it was decided to proceed with the process of finding a suitable site and developing design proposals for the Hub. This process began in February 2013. The design brief prescribed and including the key elements from the survey.
Preliminary conceptual diagrams were developed that conceived of the facility being on two levels with the service providers being located on the upper, less public level. The concept is not unique – even in the Western world. In 1935, concerned about the poor health of working-class Londoners, the Peckham Health Centre was opened in the East End of London by George Scott Willamson and Innes Hope Pearse – a husband and wife medical partnership.
They were interested in preventative social medicine. Nine hundred and fifty chosen families paid 1 shilling a week and had unlimited access to a range of activities such as physical exercise, swimming, games, workshops, dances, social events and child care. The members themselves initiated a wide range of sporting, social and cultural activities. Pearce and Crocker describe how the centre prospered until 1950 when it was superseded by the introduction of the National Health System – offering free medical services for everyone.
Tony Ward is Lecturer in Education at Toi Ohomai Institute of Technology, New Zealand. He was
Distinguished Visiting Professor in Education, Psychology and Architecture, at Miami University in Ohio from 2009-10 and Associate Professor of Education at Te Whare Wananga o Awanuiarangi, New Zealand from 2000-2006. Director of Programme Development at Te Whare Wananga o Awanuiarangi, New Zealand 2000-2006. He was a practicing architect in Britain, the USA and New Zealand until 2005.

